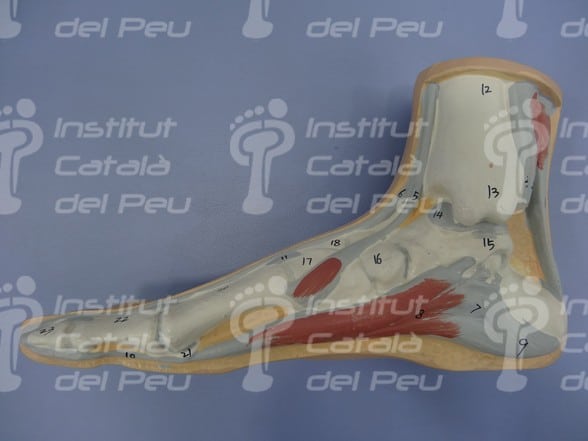
Plantar fasciitis is an inflammation of a membrane or strip of connective tissue called fascia, which runs across the bottom of foot and connects the calcaneal to the proximal phalanges.
The fascia is made up of producing cells of structural elements of the connective tissue, a fundamental liquid substance that shapes the structures and fibres of connective tissue such as the collagen, reticular or elastic fibres.
The role of facia includes the following:
- Shapinge the tissues via support, suspension and stability.
- Strength transmitter. On a muscular level, each fibre causes movement by exerting tension on those muscular fibres.
- Favouring movement by ability to stretch and deform.
- Helping to repair fibrous tissues.
- Myofascial linkages. The communication of the different bone and muscle structures is of great importance.
The most peculiar symptom of this lesion is a stabbing or intense pain in the fascia insertion (internal area of the heel), mainly after awakeing up in the morning, after a long periods of sitting down or when going up stairs. Pain is reduced when walking.
In sportspeople this pain appears after physical exercise and in the case of not taking care of the fascia at an early stage, it can restrict the practic of sport. In fact, if pain persists, its intensity increases and can covers all the plantar arch area taking a long time for such pain to disappear.
The causes of a plantar fasciitis are:
- Foot morphology (splay foot, claw foot, valgus foot, etc.).
- A pathological deambulation or mis-stepping.
- Back leg muscle loss.
- Inappropriate shoes (high heels, shoes with no stabiliser for the heel of the foo, etc.).
- Obesity.
- Sudden changes in daily routines.
It is important to know the difference between the calcaneal spur and the plantar fasciitis. The calcaneal spur is a calcification attached to the heel bone while fasciitis is caused by an inflammation not necessarily associated with a calcaneal spur.
Calcaneal spurs can be spotted by chances in X-ray and the patient may not hace experienced the sensation of pain.
The diagnosis is based on a physical test, the survey of the footprint and with the help of an X-ray, if necessary.
The treatment of plantar fasciitis at the early stages consists of anti-inflammatory drugs and analgesics as well as doing stretching exercises of the Achilles tendon, gemellus and the fascia.
The stretching of the fascia has an impact on the joints as well as on different kinds of movements.
The adhesions of the layers forming the fascia, will cause pain and limit movement. These adhesions are normally caused by either traumatisms, lesions or posturgical iatrogenia, excess of weight and hyperactivity.
The greatest stretching exercises would ideally imply those in different directions, because fascia runs in different directions across. One must consider that fascia has a lot of collagen and water that causes a more liquid viscoelastic capacity at certain points.
This will change vary depending on the temperature. For example, when we wake up in the morning, the fascia works as a solid because our temperature is lower. After warming-up exercises or wandering around for a while, the body temperature increases, therefore the fascia is transformed into a more elastic liquid.
The basic stretching exercises are as follows:
- Stretching with a towel:
We sit on the floor, with our trunk straight at 90 degrees, our legs stretched and our feet straight. We place the towel at the level of the plantar cushion (metatarsus) and the patient pulls on both sides of the towel towards himself. The traction must be kept between 15 and 30 seconds and we practice this exercise ten times.
- Use of a bottle or can as a drag roller:
Roll the bottle or the can forwards or backwards under the bare foot. Use a bottle or can takenstraight from the freeser to simultaneously apply cold.
- Stand on a one leg:
Stand on the foot affected by fasciitis, find a point of stability then stand on tiptoe.
Once on tiptoe, we slowly drop the heel until it touches the floor. Do about ten repetitions.
- Calf stretching:
Leaning hands against a bar or a wall, stretch the leg that is being treated so that the plantar surface of the foot touches the floor completely (it must not lose contact with the floor throughout the exercise).
The other leg must be slightly bended and then, we move our body foward in order to stretch the calf. Keep up the maximum tightness of the heel for ten seconds and repeat this exercise ten times.
- Stretching on a step or a sloping board:
Stand one a foot on a sloping board or step, bend the knee of the opposite extremity we want to stretch. Pressure down the heel of the extremity to be stretched for one minute and we repeat this exercise again five times.
In the case of no improvement or frequent relapses, it would be advisable for a podiatrist to examine the walk in order to consider the use of custom- made insoles that will drop the pressure in the affected area and thus will amortise impacts.
Advicing the use of type os sneaker woul not be recommendable for any patient without a podiatrist’s footprint examination.
In a more advanced stages in which pain persists and is frequently intense, we can resort to infiltrations or surgery as a final option in the case there is a chronic or a serious plantar fasciitis.
All in all, warm-up exercises and specific stretching exercises for the sole of the foot, as well as a footprint survey is a good prevention of the plantar fasciitis.
A pronated foot may cause plantar fasciitis.
A claw foot may cause plantar fasciitis.
A valgus foot may cause plantar fasciitis.
An essential flat foot may cause plantar fasciitis.
Watch for inflammation in the internal border of the heel.
The footprint survery is very important, both for prevention and treatment.
Ultrasound scanner. Severe plantar fasciitis with an intra-substance fracture.
X-ray. Watch for the appearance of a calcaneal spur.
Stretching with a towel.
Rolling with a can.
Application of a neuromuscular bandage because of plantar fasciitis and calcaneal spur.
Orthosis to be used at home in order to stretch the fascia. Watch the dorsiflexion of toes.